The Gut-Brain Connection: Why Digestive Health Matters in Therapy
Emerging research reveals that the gut-brain axis is a complex communication network linking our gastrointestinal tract and central nervous system. It plays a crucial role in emotional regulation, cognitive function, and overall mental wellbeing. For therapists and clients alike, understanding this connection opens new pathways for healing and therapeutic success.
The Science Behind the Gut-Brain Axis
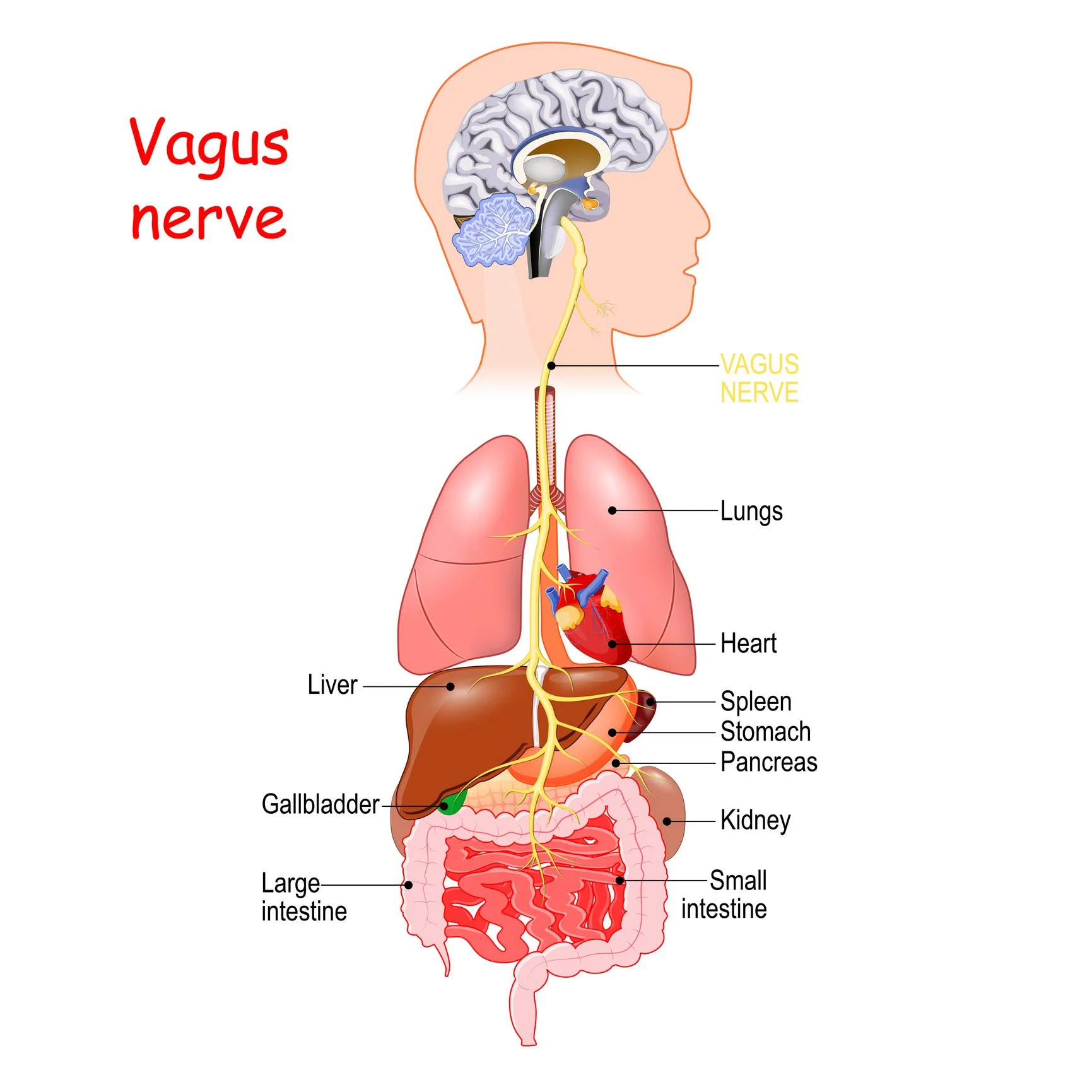
The gut-brain axis operates through multiple channels, creating a sophisticated two-way communication system. The vagus nerve serves as the primary highway, transmitting signals between the brain and digestive system in milliseconds. Meanwhile, the enteric nervous system—often called the "second brain"—is a complex network of millions of neurons embedded in the lining of the gastrointestinal system, beginning in the esophagus and extending down to the anus.
This intricate network means that what happens in your gut directly influences your mental state. The gut microbiome, consisting of trillions of bacteria, fungi, and other microorganisms, produces neurotransmitters including serotonin, dopamine, and GABA. About 90% of the body's serotonin—a key neurotransmitter for mood regulation—is produced in the gut, not the brain.
How Digestive Health Impacts Mental Health
Research consistently demonstrates strong correlations between gut health and psychological wellbeing. Individuals with irritable bowel syndrome (IBS) show significantly higher rates of anxiety and depression compared to the general population. Similarly, those experiencing chronic digestive inflammation often report increased symptoms of mood disorders, cognitive fog, and emotional dysregulation.
The microbiome's influence extends beyond neurotransmitter production. Beneficial bacteria help regulate the hypothalamic-pituitary-adrenal (HPA) axis, our body's primary stress response system. When gut bacteria are imbalanced—a condition called dysbiosis—it can trigger chronic inflammation, disrupt sleep patterns, and impair the body's ability to manage stress effectively.
Implications for Therapeutic Practice
Integrating awareness of digestive health can enhance therapeutic outcomes significantly. When clients struggle with persistent anxiety, depression, or emotional volatility despite consistent therapeutic work, exploring gut health often reveals contributing factors that purely psychological or emotional approaches might miss.
Therapists increasingly recognize that trauma and chronic stress don't just affect the mind—they alter gut bacteria composition and digestive function. This creates a cycle where psychological distress disrupts gut health, which in turn exacerbates mental health symptoms. Breaking this cycle requires addressing both psychological and physiological components.
Practical Strategies for Supporting Gut Health in Therapy
Incorporating gut health awareness into therapeutic practice doesn't require medical training, but it does involve recognizing the interconnected nature of physical and mental wellbeing. Therapists can explore with clients how digestive symptoms correlate with emotional states, stress levels, and therapeutic progress.
Encouraging clients to maintain a mood and digestion journal often reveals surprising patterns. Many discover that certain foods trigger both digestive discomfort and increased anxiety, or that periods of high stress consistently precede both emotional difficulties and gastrointestinal symptoms.
Stress management techniques take on new significance when viewed through the gut-brain lens. Practices like deep breathing, progressive muscle relaxation, and mindfulness meditation don't just calm the mind—they activate the parasympathetic nervous system, promoting healthy digestion and supporting beneficial gut bacteria.
Nutritional Considerations for Mental Health
While therapists shouldn't provide specific dietary advice without appropriate training, understanding basic nutrition principles helps contextualize client experiences. Diets high in processed foods, sugar, and artificial additives can disrupt gut bacteria balance and increase inflammation, potentially undermining therapeutic progress.
Conversely, foods rich in prebiotics and probiotics—such as yogurt, kefir, sauerkraut, and fiber-rich vegetables—support beneficial bacteria growth. Omega-3 fatty acids found in fish, walnuts, and flaxseeds have anti-inflammatory properties that benefit both gut and brain health.
Moving Forward: A Holistic Perspective
The gut-brain connection reminds us that mental and emotional health exist within the broader context of overall wellbeing. Acknowledging the role of digestive health opens new possibilities for healing and growth. It enriches our understanding of the complex factors that influence mental health and recovery. By considering the whole person, we can offer more comprehensive, effective support.
As research continues to illuminate the sophisticated relationship between our digestive and nervous systems, the future of mental health treatment will likely become increasingly integrative. For now, simply recognizing that our gut health and mental health are inextricably linked represents an important step toward more holistic, effective therapeutic practice.
References
Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701-712.
Foster, J. A., & McVey Neufeld, K. A. (2013). Gut-brain axis: How the microbiome influences anxiety and depression. Trends in Neurosciences, 36(5), 305-312.
Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut/brain axis and the microbiota. Journal of Clinical Investigation, 125(3), 926-938.
Moloney, R. D., Desbonnet, L., Clarke, G., Dinan, T. G., & Cryan, J. F. (2014). The microbiome: Stress, health and disease. Mammalian Genome, 25(1-2), 49-74.
Petra, A. I., Panagiotidou, S., Hatziagelaki, E., Stewart, J. M., Conti, P., & Theoharides, T. C. (2015). Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clinical Therapeutics, 37(5), 984-995.
Rhee, S. H., Pothoulakis, C., & Mayer, E. A. (2009). Principles and clinical implications of the brain-gut-enteric microbiota axis. Nature Reviews Gastroenterology & Hepatology, 6(5), 306-314.
Sudo, N., Chida, Y., Aiba, Y., Sonoda, J., Oyama, N., Yu, X. N., ... & Koga, Y. (2004). Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. Journal of Physiology, 558(1), 263-275.
Tillisch, K., Labus, J., Kilpatrick, L., Jiang, Z., Stains, J., Ebrat, B., ... & Mayer, E. A. (2013). Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology, 144(7), 1394-1401.